Dr. Joseph Giancola joined U.S. Dermatology Partners, formerly Southwest Skin Specialists, in 1997. After attaining his undergraduate degree from Creighton University in 1986, Dr. Joseph Giancola graduated with honors from the University of Missouri-Columbia School of Medicine in 1990. His postgraduate training included an internship and residency in internal medicine at Good Samaritan Regional Medical Center in Phoenix and a residency in dermatology at the University of Arizona. He completed a Mohs surgical fellowship with Dr. George Hruza at the Laser and Dermatologic Surgery Center in St. Louis in 2001.
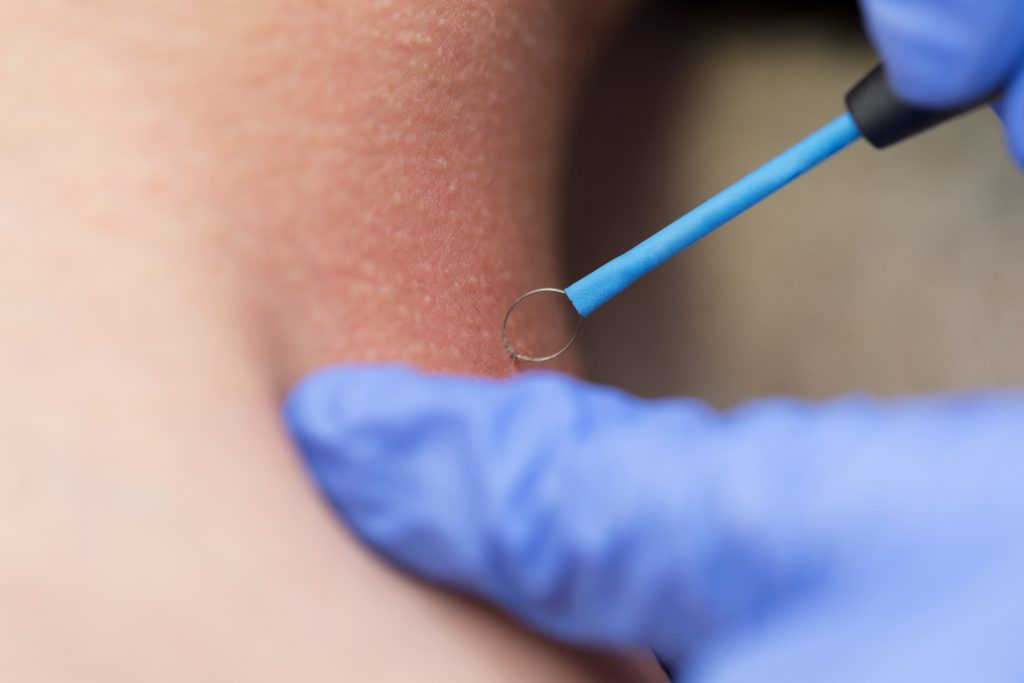
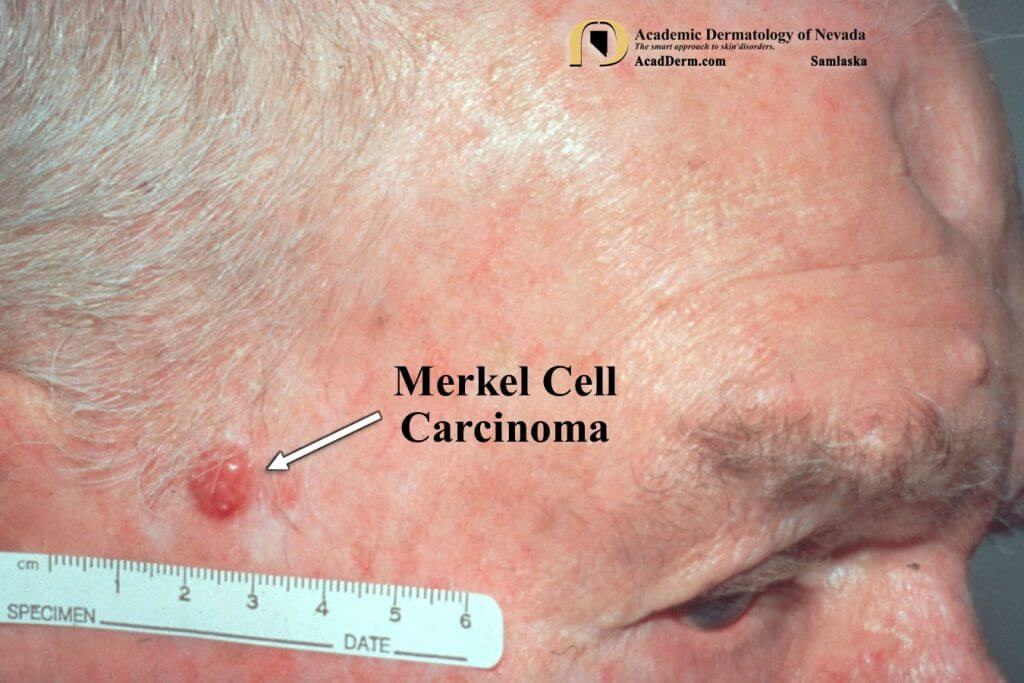
Dr. Joseph Giancola specializes in Mohs surgery and cutaneous oncology. In addition to being an associate professor at Creighton University School of Medicine, he lectures at the University of Arizona College of Medicine and volunteers at the dermatology clinic at St. Vincent De Paul in Phoenix.
Dr. Giancola provides dermatology care to patients in Phoenix, Arizona.
Specialties and Affiliations
- Fellow, American Academy of Dermatology
- Fellow, American College of Mohs Surgery
- Member, American Society of Dermatologic Surgery
- Member and past president, Phoenix Dermatologic Society
- Member and past executive council member, Arizona Dermatology and Dermatologic Surgery Society
Badges & Awards
- PHOENIX Magazine’s Top Doctors Honor
- Scottsdale Magazine’s Top Doctors Honor