Leon Chen, MD is a board-certified dermatologist and a fellowship-trained Mohs surgeon who earned his Medical Doctorate from the University of Texas McGovern Medical School at Houston. He completed his dermatology residency training at the MD Anderson Cancer Center/University of Texas McGovern Medical School combined program and his Micrographic Surgery and Dermatologic Oncology (Mohs) fellowship at MD Anderson Cancer Center. He was the winner of the Review Article Incentive Program awarded by the American Society for Dermatologic Surgery (ASDS) during his time as a dermatology resident. His fellowship training focused on Mohs micrographic surgery, advanced reconstruction, and clinical research in cutaneous oncology. He was the sub-investigator of various clinical trials that evaluated the use of a hedgehog pathway inhibitor and immunotherapy for advanced nonmelanoma skin cancer. Dr. Chen’s deep passion for skin cancer has led him to author more than 30 peer-reviewed research manuscripts and numerous book chapters. His research has been presented at national and international dermatology meetings. He is also the editor of the textbook Basal Cell Carcinoma: Advances in Treatment and Research.
Dr. Chen is certified by the American Board of Dermatology and a Fellow of the American College of Mohs Surgery. He is a member of the American Academy of Dermatology, the American Society for Dermatologic Surgery, the American College of Mohs Surgery, the American Medical Association, and the Texas Medical Association.
In his free time, Dr. Chen enjoys spending time with his wife, Patty, and two young boys, Levi and Luke. He is also an avid sports fan who follows the Rockets, the Texans, the Astros as well as sports teams from his alma mater Texas Longhorns.
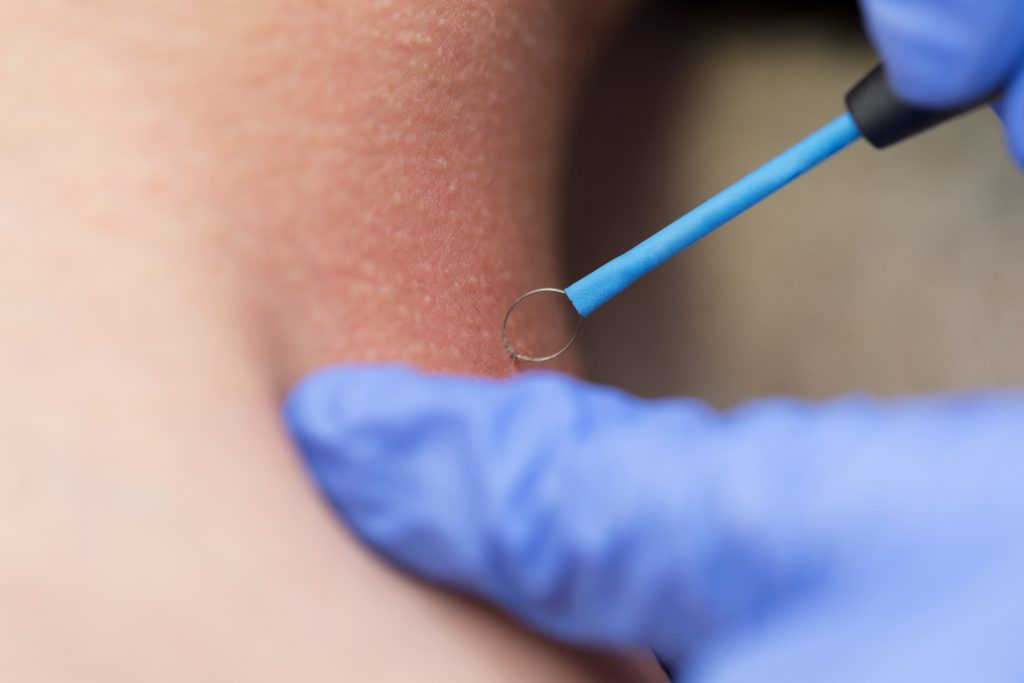
Dr. Leon Chen performs Mohs Surgery in our Houston-area offices at U.S. Dermatology Partners Medical District, U.S. Dermatology Partners Sugar Land, and U.S. Dermatology Partners Pasadena.
Specialties and Affiliations
- American Board of Dermatology
- American Academy of Dermatology
- American College of Mohs Surgery
- American Society for Dermatologic Surgery
- American College of Mohs Surgery
- American Medical Association
- Texas Medical Association
Featured Blogs
- 42 U.S. Dermatology Partners Physicians Recognized by 2024 Super Doctors® Awards
- Super Doctors Recognizes 16 Dermatology Partners Physicians as Rising Stars in Peer-Nominated Award
- Super Doctors 2023 Recognizes 43 U.S. Dermatology Partners Physicians in Peer-Nominated Award
- Texas Monthly Super Doctors 2023 Recognizes 18 U.S. Dermatology Partners Physicians as Rising Stars in Peer-Nominated Award
- Texas Monthly Super Doctors 2022 Recognizes 14 U.S. Dermatology Partners Physicians as Rising Stars in Peer-Nominated Award
- U.S. Dermatology Partners Sugar Land Will Now Offer Mohs Surgery
- U.S. Dermatology Partners Welcomes Fellowship-Trained Mohs Surgeon, Leon Chen, MD to Houston Medical District Location
- What Are Skin Tags & What Can I Do About Them?
- Mole Removal: What to Know Before You Visit a Dermatologist
- Caring for Your Skin After Mohs Surgery: The Importance of Nonchemical Sunscreens
- What to Expect During and After Mohs Surgery
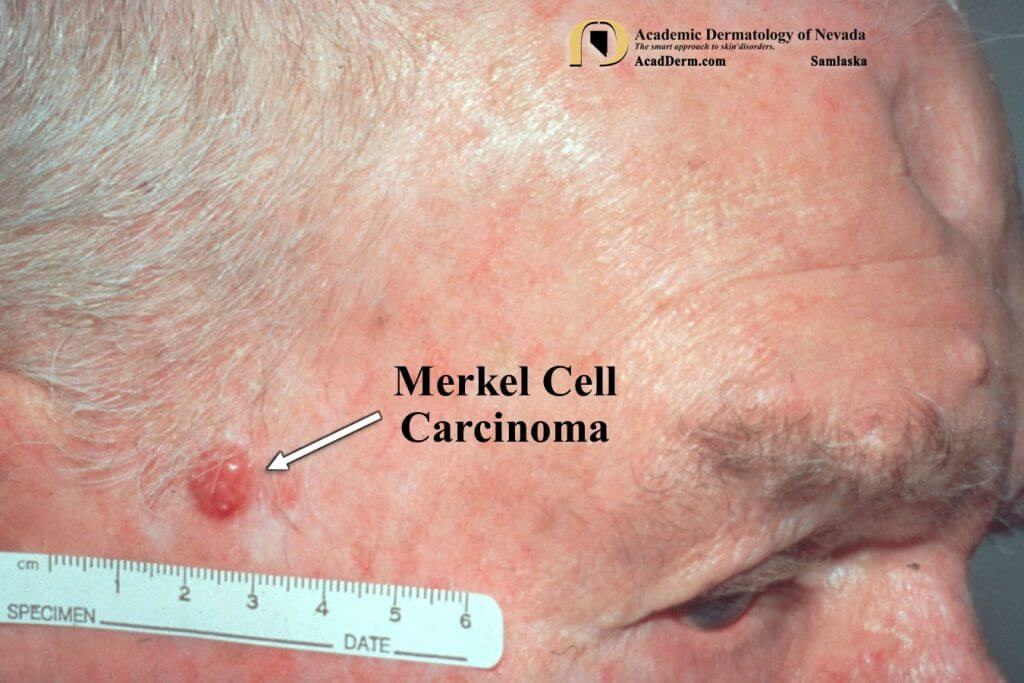
- What Does Skin Cancer Look Like?