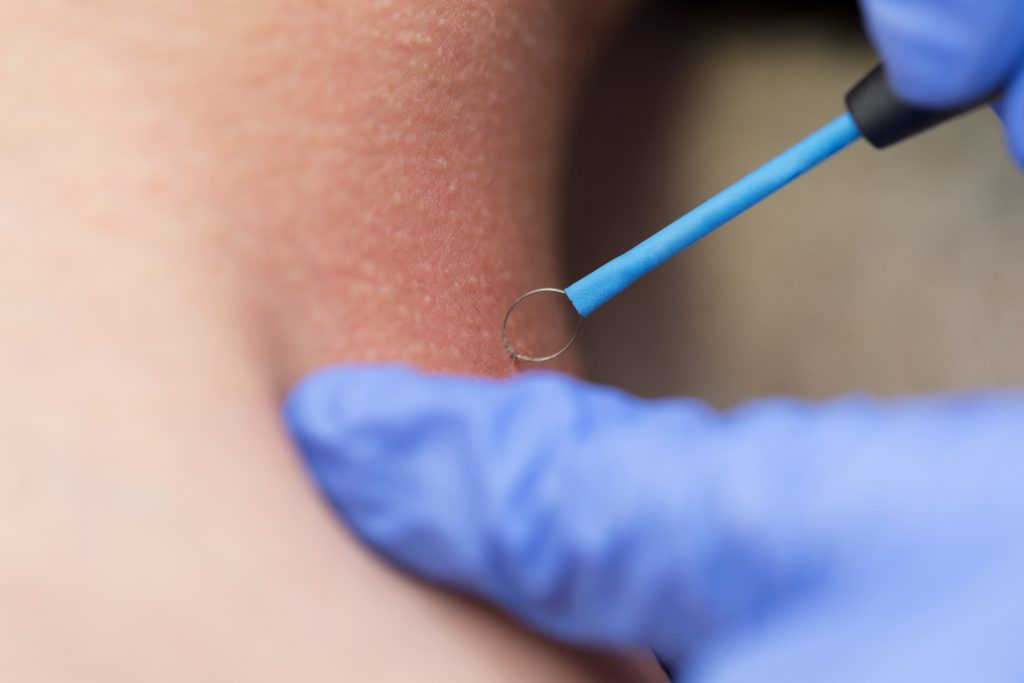
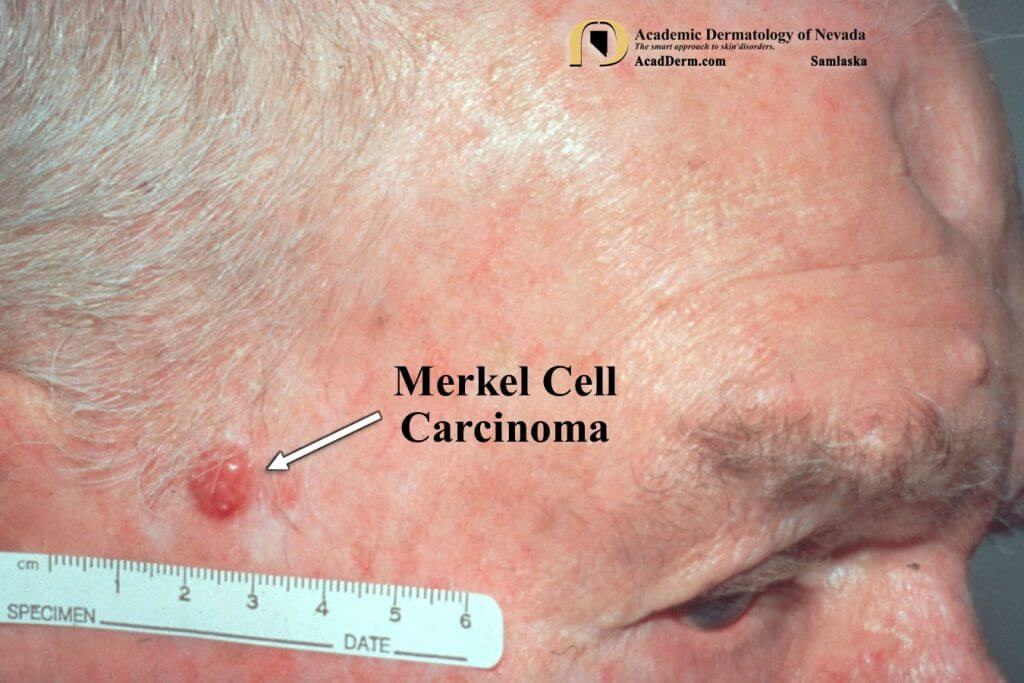
Dr. Nathalie Zeitouni is a nationally recognized Fellowship-Trained Mohs surgeon with experience in the multidisciplinary care of cutaneous oncology patients. She is currently a Professor of Dermatology at the University of Arizona COM Phoenix, and adjunct Professor of Oncology at Roswell Park Comprehensive Cancer Center (RPCCC) in Buffalo, NY. Her approach to care includes prevention, treatment, and research in the areas of Mohs surgery, skin cancer, dermatologic surgery, and melanoma. She is a national leader in the field of photodynamic therapy (PDT) and known for her work with the rare forms of skin cancer, such as Merkel cell carcinoma, Dermatofibrosarcoma protuberans, and Extramammary Paget’s disease. She is currently a board member of the American College of Mohs surgery and of the International Society of Dermatologic Surgery. Additionally, Dr. Zeitouni is a former board member of The International Transplant Skin Cancer Collaborative (ITSCC) and has significant expertise in the treatment of organ transplant patients who have a much higher risk of developing skin cancers.
As a recipient of numerous NCI and industry grants, Dr. Nathalie Zeitouni has a rich history researching the various aspects of skin cancers. She has published more than 100 peer-reviewed manuscripts and book chapters and given numerous national and international presentations.
Prior to joining U.S. Dermatology Partners, formerly Medical Dermatology Specialists Phoenix, she was the Section Leader at the University of Arizona Cancer Center at DHMC and held the position of Vice Chief of Dermatology at the University of Arizona in Tucson, Arizona. Her distinguished career also includes serving as Chair of the Department of Dermatology and Director of the Mohs Surgery Fellowship at RPCCC in Buffalo, NY.
Additional Languages
-
French
Specialties and Affiliations
- American Board of Dermatology
- American Academy of Dermatology