Hives Treatments from U.S. Dermatology Partners
What Are Hives?
If you’re dealing with the itchy, inflamed, painful skin condition called hives, it may be time to call U.S. Dermatology Partners for help. Hives can be very uncomfortable, but recognizing the warning signs and taking appropriate actions to care for your skin can be important to quickly relieve these symptoms and get back to feeling your best. Keep reading to learn more about what causes hives and how your dermatologist can treat this condition.
Find This Service Near You
What Are Hives?
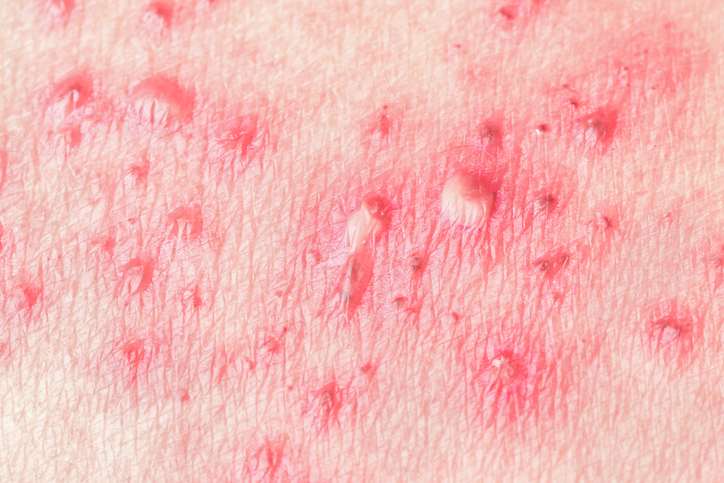
Hives appear as a red, raised, itchy rash on the skin
Hives, known by the medical name urticaria, can develop in response to allergen exposure or be a chronic skin condition. Hives are most often due to an allergic reaction which causes the body to release a protein called histamine. This protein causes our capillaries to leak fluid, which can accumulate below the skin, causing a rash. Hives can appear seemingly at random and clear up within hours or days. They can also change in size or shape, and hives may even clear up in one area and reappear in a different location. The good news is that hives, while irritating and possibly painful, are typically not a threat to your overall health, and they will almost always clear up on their own with appropriate treatment.
Are there Different Types of Hives?
There are two types of hives: Acute Urticaria & Idiopathic Urticaria
 Acute Urticaria
Acute Urticaria
The first, acute urticaria, is what most people think of when they hear the word hives. This the type of hives that develop due to a reaction to an environmental allergen or irritant, including an allergic reaction to foods or medications, irritation caused by sunlight exposure or friction, and a range of other issues. In most cases, this type of hives will clear up within a few days or weeks.
Idiopathic Urticaria
The second type of hives, idiopathic urticaria, are chronic and more severe.
Flare-ups in this condition may last for more than six weeks or recur regularly throughout the individual’s life with no apparent underlying cause. Unlike acute urticaria, the chronic form may require the attention of a professional dermatologist to help you treat the immediate symptoms and combat future flare-ups.
Who Is at Risk for Hives?
In many cases, the underlying stimulus for the development of hives is unclear, and just about anyone can develop acute hives from time to time. However, idiopathic or chronic hives are more likely for individuals with a family history of hives; and those who have experienced a previous allergic reaction have a greater risk of developing hives in the future. Allergies, food additives and preservatives, infections, and certain medications or medical treatments can also trigger hives. While allergens and irritants like these are often associated with hives, the direct catalyst for a flare-up is not always clear. Because acute urticaria clears up on its own and is relatively harmless, advanced allergy testing and other diagnostic measures are not typically taken to determine the exact cause of hives. For individuals suffering from chronic hives, more advanced testing may be recommended to help the dermatologist determine the underlying causes of chronic hives in order to develop an effective treatment plan.
What are the Symptoms of Hives?
A breakout of hives usually involves rashes, made up of swollen red bumps called wheals. These wheals most often appear on the face, arms, hands, feet, or legs, but can develop anywhere on the body. These individual bumps or patches can grow, change in shape, and rashes may even change locations. The area affected by the rash may be itchy, swollen, or painful. During a flare-up of hives, individuals may also experience swelling in the lips, throat, or eyes.
What are the Treatment Options for Hives?

For symptoms of more severe or chronic hives, persisting for longer than six weeks, you should schedule an appointment with your dermatologist at U.S. Dermatology Partners. In these cases requiring medical attention, your doctor may prescribe a high-dose oral corticosteroid or other immunosuppressant medications, prescription antihistamines, or biologic immunomodulators to stop the hives in the short term. Long term interventions may involve more advanced diagnostic screenings and tests to determine the underlying cause of hives and help you avoid these triggers and prevent future flare-ups.
Can Hives be Prevented?
The best way to prevent hives is to avoid known triggers, such as certain foods, medications, or extreme temperatures. In addition to learning and avoiding the factors that trigger flare-ups, individuals who struggle with chronic hives may also want to take allergy medicines each day to reduce their risk for flare-ups and avoid severe symptoms. Once you notice signs of hives, it’s important to address these symptoms right away to prevent more severe or prolonged flare-ups.
Specifically, you should take the following steps when you have hives:
- Avoid scratching the skin
- Wear loose-fitting clothing
- Use cold compresses, cool baths, and anti-itch creams to soothe skin
- Apply sunscreen before going outdoors
- Avoid spending too long in overly warm or humid environments
Is Hives Treatment Permanent?

Additionally, being prepared to respond quickly when you notice the first signs of a hives flare-up, can ensure you don’t struggle with painful, itchy rashes for weeks at a time. Instead, your dermatologist at U.S. Dermatology Partners will work with you to keep your skin healthy and provide effective treatment to minimize the symptoms of hives. In addition to working with a dermatologist for effective hives therapy and skin care maintenance plans, you may also want to make notes of any foods, weather conditions, cleaning products, cosmetics, medications, chemicals you’re exposed to, and other factors that may be associated with a flare-up. If you notice common elements between two or more hives flare-ups, you may want to consider eliminating the triggering product from your environment.
*Results may vary by individual


 Acute Urticaria
Acute Urticaria